Recurrent Miscarriages: When to Seek Specialist Help
Introduction
Experiencing one miscarriage is emotionally draining, but going through multiple losses can be devastating. Recurrent miscarriage, defined as the loss of two or more consecutive pregnancies, affects about 1% of couples. Understanding when to seek specialist help can be a crucial step toward finding answers and exploring treatment options. This article discusses common causes, available treatments, and the path to a healthy pregnancy after recurrent miscarriages.
What Is Recurrent Miscarriage?
Medical Definition
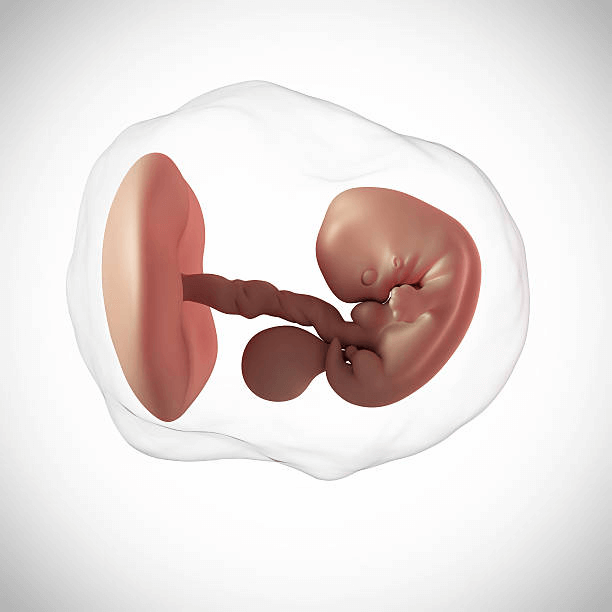
Recurrent miscarriage (also called recurrent pregnancy loss) is the loss of two or more pregnancies before the 20th week. While one miscarriage is relatively common, multiple losses may signal underlying issues that require medical attention.
Prevalence
- About 1 in 100 couples experience recurrent miscarriages.
- The risk increases with maternal age, especially after 35.
Risk Factors
- Age (women over 35)
- Previous pregnancy loss
- Chronic health conditions (e.g., diabetes, thyroid disorders)
- Lifestyle factors (smoking, drug use)
Common Causes of Recurrent Miscarriages
1. Genetic Factors
- Chromosomal Abnormalities: Genetic issues, such as translocations, may prevent a healthy pregnancy.
- Parental Karyotyping: Testing both partners’ chromosomes can detect inherited genetic problems.
2. Hormonal Imbalances
- Low Progesterone: Essential for maintaining the uterine lining.
- Thyroid Disorders: Hypothyroidism and hyperthyroidism increase the risk of miscarriage.
3. Anatomical Issues
- Uterine Abnormalities: Conditions like fibroids, septate uterus, or scar tissue can disrupt implantation.
- Cervical Incompetence: A weak cervix may cause pregnancy loss in the second trimester.
4. Autoimmune Disorders
- Antiphospholipid Syndrome (APS): An immune system disorder causing blood clots that interfere with the placenta.
- Lupus: Can cause inflammation, affecting the pregnancy environment.
5. Lifestyle Factors
- Smoking and Alcohol: Both are linked to a higher risk of miscarriage.
- Obesity and Poor Nutrition: Affect hormone regulation and pregnancy outcomes.
For tips on managing pregnancy symptoms and appetite, read this guide on food aversions during pregnancy.
Signs You Need to See a Specialist
Consider seeing a fertility specialist if:
- You’ve had two or more consecutive miscarriages.
- You’re over 35 years old.
- You have a history of medical conditions like diabetes, PCOS, or thyroid disorders.
- You’ve experienced pregnancy loss after 12 weeks, which may indicate cervical or uterine issues.
- Previous pregnancies were complicated by preterm labor or stillbirth.
Types of Specialists for Recurrent Miscarriages
- Obstetricians: Experts in high-risk pregnancies.
- Reproductive Endocrinologists: Specialists in fertility treatments.
- Genetic Counselors: Help assess genetic risks and recommend testing.
- Maternal-Fetal Medicine (MFM) Specialists: Offer advanced pregnancy monitoring and care.
Diagnostic Tests and Procedures
Specialists may recommend the following tests:
- Blood Tests: To check for hormonal imbalances, clotting disorders, and autoimmune conditions.
- Ultrasound: To assess uterine abnormalities and fetal development.
- Hysteroscopy: A procedure to inspect the uterus for scarring or fibroids.
- Karyotyping: Genetic testing for both partners.
Treatment Options Available
- Hormonal Therapy: Progesterone or thyroid hormone replacement.
- Surgery: To correct uterine abnormalities like fibroids or septate uterus.
- Medications: Blood thinners for clotting disorders like APS.
- Fertility Treatments: In vitro fertilization (IVF) with genetic testing can improve outcomes.
Lifestyle Changes to Support Pregnancy
- Healthy Diet: Focus on nutrient-dense foods like fruits, vegetables, and lean proteins.
- Moderate Exercise: Walking or prenatal yoga can improve physical health.
- Avoid Harmful Substances: Quit smoking, alcohol, and recreational drugs.
- Manage Stress: Try mindfulness, meditation, and counseling.
Learn more about maintaining a healthy lifestyle during early pregnancy from this first-trimester survival guide.
Coping With the Emotional Toll
Recurrent miscarriage can cause deep emotional pain, anxiety, and depression. Consider these coping strategies:
- Therapy: Seek individual or couples counseling.
- Support Groups: Connect with others who have experienced similar losses.
- Partner Support: Open communication with your partner is essential.
FAQs About Recurrent Miscarriages
1. How many miscarriages before seeing a specialist?
See a specialist after two or more consecutive miscarriages.
2. Can recurrent miscarriages be treated?
Yes, treatment depends on the underlying cause, including medications, surgery, and fertility therapies.
3. Are recurrent miscarriages genetic?
They can be. Genetic testing helps identify chromosomal issues.
4. What tests are done for recurrent miscarriage?
Blood tests, ultrasounds, hysteroscopies, and genetic screening are common.
5. Can I have a healthy pregnancy after recurrent miscarriages?
Many women have successful pregnancies after receiving appropriate treatment and support.
Conclusion
Recurrent miscarriages are emotionally and physically challenging, but modern medicine offers hope through advanced diagnostic testing, personalized treatments, and supportive care. Don’t hesitate to seek help from a specialist. With the right care, many couples overcome pregnancy loss and experience the joy of a healthy baby.