Mastitis & Clogged Ducts: Causes, Symptoms, Solutions

As a nursing mom, you might face challenges like mastitis and clogged milk ducts. Mastitis can be uncomfortable and make breastfeeding hard. It’s key to know about these issues to prevent and treat them well.
Many moms deal with plugged ducts, breast infections, and thrush. These problems can make breastfeeding tough.
Breastfeeding challenges like mastitis and clogged ducts are common. Knowing the symptoms and causes helps you prevent and treat them. Being informed lets you keep breastfeeding and give your baby the nutrients they need.
Key Takeaways
- Understanding mastitis and clogged milk ducts is key for prevention and treatment.
- Mastitis symptoms can be hard to tell apart from plugged ducts.
- Getting help from lactation consultants can greatly improve breastfeeding.
- Wearing a supportive bra can lower the risk of clogged ducts.
- Early treatment can cut down breastfeeding problems by up to 50%.
- Keeping milk flow going and gentle breast massage can prevent clogged ducts.
- Wearing loose clothes and regular breastfeeding can ease breast pressure.
Understanding Mastitis and Clogged Milk Ducts: Prevention and Treatment
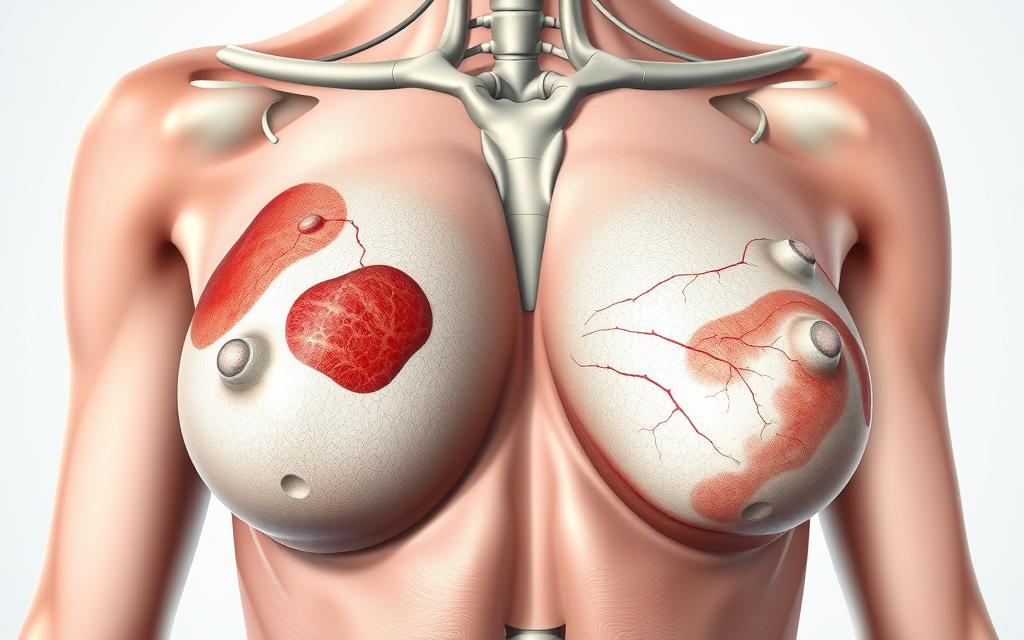
Mastitis and clogged milk ducts are common problems for breastfeeding moms. Knowing what mastitis definition and clogged duct causes are can help. Studies show up to 20% of breastfeeding moms get mastitis at some point.
Symptoms of mastitis include fever, pain in one area, and swelling. Clogged milk ducts feel like a hard, sore lump. It’s important to empty the breast often to fight inflammation and avoid problems.
- Practice proper latch and positioning
- Frequently feed or express milk
- Avoid tight-fitting bras or clothing
By knowing the causes and symptoms of mastitis and clogged milk ducts, moms can prevent and treat them. This ensures a healthy and successful breastfeeding journey.
Early Warning Signs to Watch For
It’s important to know the mastitis warning signs to get treatment early. Nursing moms should look out for a sore lump in the breast, flu-like symptoms, and changes in the breast’s look. These can include redness or swelling.
Some breastfeeding challenges that might mean mastitis or clogged ducts are a low fever, plugged ducts, or a warm breast. It’s key to watch for these signs and get help if they don’t go away or get worse.
Some key signs to watch for include:
- A tender or sore lump in the breast
- Flu-like symptoms, such as fever and chills
- Changes in the breast’s appearance, such as redness or swelling
- A low fever, typically less than 101.3°F (38.5°C)
Knowing these early signs helps nursing moms get help fast. This can prevent serious problems and make breastfeeding healthier.
Common Causes of Mastitis
Mastitis is a common issue for breastfeeding moms, affecting 10% to 33% of them. Knowing the mastitis causes helps moms prevent it. Issues like poor latch, blocked ducts, and bacterial infections are common reasons.
Good breastfeeding techniques like a proper latch can prevent mastitis. Also, expressing milk or feeding on demand can help. Knowing risk factors like a history of mastitis or sore nipples helps prevent it.
Some key factors that contribute to mastitis include:
- Poor latch and feeding issues
- Blocked milk ducts
- Bacterial infections
- Pressure on the breast, such as from a tight bra or seat belt
- Stress and fatigue
By understanding mastitis causes and taking steps to prevent it, moms can have a healthier breastfeeding experience.
Risk Factors for Developing Clogged Ducts
It’s important for breastfeeding moms to know about clogged duct risk factors. Severe engorgement, breastfeeding on just one side, skipping feedings, or tight clothing can cause clogs. Knowing these clogged duct risk factors helps moms prevent them. They can do this by expressing milk often and wearing loose clothes.
Getting the right breastfeeding support is also key. This means using the right latch and feeding methods, and expressing milk regularly. By being aware and proactive, moms can lower their chance of clogged ducts. This ensures a smooth and healthy breastfeeding journey.
- Severe engorgement
- Regularly breastfeeding on only one breast
- Skipping feedings
- Pressure against the milk ducts
Understanding and preventing these risk factors is vital. It helps breastfeeding moms have a successful and healthy experience. With the right breastfeeding support, they can enjoy a fulfilling journey.
The Connection Between Mastitis and Breast Health
Mastitis can affect breast health in many ways. It’s important for nursing moms to know this. Lactation support is key in preventing and managing mastitis. It helps keep milk supply healthy and lowers the risk of problems.
Good breast health and preventing mastitis involve several steps. These include:
- Regular breastfeeding or pumping to prevent milk stasis
- Proper latch and feeding techniques to avoid nipple trauma
- Seeking medical attention if symptoms persist for more than 24 hours
Mastitis can also impact milk supply. Untreated, it can lead to less milk. But, with the right treatment and lactation support, moms can keep breastfeeding. The American Academy of Pediatrics suggests exclusive breastfeeding for 6 months. Then, continue for at least 1 year or longer if both mom and baby want to.
Long-term, mastitis can raise the risk of breast abscesses or scarring. So, it’s vital to focus on breast health. If mastitis symptoms show up, get medical help right away. Knowing how mastitis affects breast health helps moms stay proactive. This ensures a successful breastfeeding journey.
Medical Treatment Options
Medical experts often suggest a mix of antibiotics, pain relievers, and lymphatic drainage for mastitis. A 10-day antibiotic course is common to fight the infection. Pain relievers like acetaminophen or ibuprofen can also help with pain and fever.
Nursing moms should talk to their doctor to find the right treatment. This depends on how bad the symptoms are and any risks. Sometimes, a hospital stay is needed for the best care and to avoid problems.
It’s safe to keep breastfeeding during mastitis. It can help clear the infection. But stopping suddenly can make symptoms worse.
Some important tips for mastitis treatment include:
- Express a small amount of milk by hand before breastfeeding to help with latching, even if the breast is swollen
- Breastfeed on the affected side first when the baby is hungry and sucking hard
- Rest as much as you can and drink lots of water to stay hydrated
- Get help from a lactation consultant for breastfeeding support
Knowing about mastitis treatment helps nursing moms face breastfeeding challenges. It’s important to see a doctor if symptoms don’t get better or get worse. Untreated mastitis can lead to serious issues like abscesses or stopping breastfeeding altogether.
Natural Remedies and Home Care Strategies
For breastfeeding moms with mastitis, there are many natural ways to feel better. These methods can work alongside doctor’s advice to help you heal and keep breastfeeding strong.
Lymphatic drainage and reverse pressure softening can help with swelling and milk flow. Using ice or cold packs can also ease pain and reduce swelling.
Eating well is key for breastfeeding support. Foods high in vitamin C boost your immune system and health. Drinking lots of water is also important to keep your milk supply up.
Castor oil packs and probiotics might also help you recover from mastitis. But remember, these natural remedies should not replace medical care. If your symptoms don’t get better or get worse, you need to see a doctor.
Prevention Strategies for Nursing Mothers
As a nursing mother, it’s key to prevent mastitis. Mastitis prevention means using the right breastfeeding techniques, making lifestyle changes, and knowing the risks. Understanding mastitis causes and taking steps to prevent it can lower your risk.
About 10% of breastfeeding moms might get mastitis. But, by breastfeeding often, expressing milk regularly, and keeping breasts clean, you can lower your risk. It’s best to breastfeed at least 8 to 12 times in 24 hours.
Here are some ways to prevent mastitis:
- Frequent and effective milk removal
- Proper breast hygiene, including keeping nipples clean and dry between feedings
- Avoiding tight clothing or pressure against the milk ducts
- Maintaining a healthy lifestyle, including a balanced diet and adequate rest
By using these breastfeeding techniques and making lifestyle changes, you can prevent mastitis. It’s also important to know the signs of mastitis, like redness, pain, or tenderness. If you notice these symptoms, get medical help right away.
When to Seek Immediate Medical Attention
As a breastfeeding mom, knowing when to act fast is key. Mastitis can be painful and hard to handle. It usually gets better with antibiotics and home care. But, some cases need urgent medical help.
If you have a high fever, chills, or trouble breathing, go to the emergency room. These signs mean you need help right away.
A fever of 100.4°F (38°C) or higher is a clear sign to see a doctor. Also, if you feel a warm, swollen lump in your breast, get medical help fast. These signs could mean you have a mastitis emergency.
Some warning signs that mean you need to go to the doctor right away include:
- Severe pain or swelling in the breast
- High fever or chills
- Difficulty breathing
- Red streaks extending from the breast towards the chest or arms
Having trouble with breastfeeding, like clogged milk ducts, can lead to mastitis. Make sure to empty your breasts fully when you’re breastfeeding. This can help avoid clogged ducts and mastitis.
When you need medical help, find a doctor who knows about breastfeeding. They can give you the right care and support to deal with mastitis and breastfeeding issues.
Impact on Breastfeeding Journey and Emotional Well-being
Mastitis can really affect a mother’s breastfeeding and emotional health. The pain and stress from mastitis can make it hard to keep breastfeeding. This can lead to feelings of frustration and sadness. But, with the right emotional support, mothers can get through these tough times and keep breastfeeding healthy.
Studies show that breastfeeding can help lower postpartum depression. But, mastitis and other breastfeeding problems can increase depression and anxiety. It’s key for mothers to have a strong support system, like family, friends, and healthcare professionals, to help them through these hard times.
Here are some ways to deal with the emotional side of mastitis and breastfeeding issues:
* Look for help from a lactation consultant or breastfeeding support group.
* Take care of yourself with stress-reducing activities like meditation or deep breathing.
* Connect with other moms who have faced similar problems.
* Make sure to take care of your mental health and seek help if you need it.
By understanding the emotional effects of mastitis and breastfeeding challenges, mothers can prepare better. They can also find the support they need to have a positive breastfeeding experience.
Conclusion: Maintaining Healthy Breastfeeding Practices
Keeping up with healthy breastfeeding practices is key to avoiding mastitis and making breastfeeding a success. Moms can lower their risk by keeping their breasts clean, nursing often, and pumping milk regularly. If they notice any lasting symptoms, they should get medical help right away.
By focusing on their breast health and getting help when needed, moms can beat breastfeeding hurdles. Experts say breastfeeding for at least six months is best, but many stop early due to issues. With the right approach and support, moms can keep breastfeeding healthy and enjoy it with their babies.






