Comprehensive Guide to Bacterial Vaginosis (BV) in Pregnancy
Understanding Bacterial Vaginosis
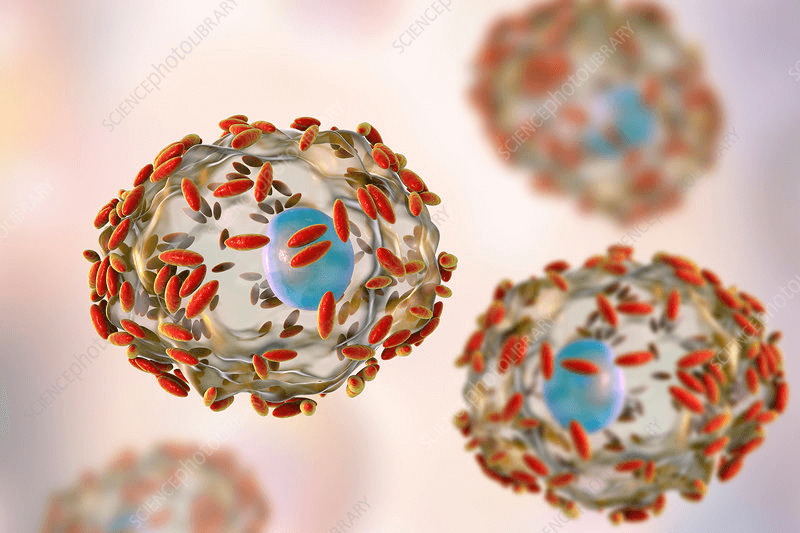
Bacterial vaginosis (BV) is a common vaginal infection caused by an imbalance of bacteria. Approximately one in eight women experience BV during pregnancy. This condition arises when the normal, healthy bacteria, known as lactobacilli, are reduced, making way for harmful bacteria to proliferate.
Lactobacilli help maintain vaginal health by producing lactic acid, which keeps the vaginal environment slightly acidic, inhibiting the growth of harmful bacteria. In cases of BV, the reduced acidity allows other bacteria to flourish, leading to infection.
While BV is a common cause of unusual vaginal discharge, it’s important to note that increased discharge is also a normal part of pregnancy. Therefore, don’t immediately assume you have BV based on discharge alone.
Identifying Bacterial Vaginosis
Many women with BV may not exhibit any symptoms, making it possible to have the infection without knowing it. In some cases, women only discover they have BV through routine vaginal swabs done for other reasons. Testing for BV is not standard practice because universal screening and treatment have not been shown to significantly benefit most pregnancies.
For those who do experience symptoms, they may include a thin, white or gray discharge with a noticeable fishy odor, especially after sex. If you suspect you have BV, it’s essential to consult your doctor, who can perform a test on a sample of your vaginal discharge. Results may be available immediately or could take up to a week.
Also read: Understanding Vaginal Discharge During Early and Late Pregnancy
The Impact of BV on Pregnancy
For most women, having BV during pregnancy is unlikely to cause complications, especially if they don’t have symptoms. However, if BV is detected and symptoms are present, treatment is necessary to avoid potential complications, particularly if you’ve had issues in previous pregnancies.
Complications associated with untreated BV symptoms include:
- Premature labor
- Late miscarriage
- Postpartum uterine infection
If you’ve had a premature birth before, your healthcare provider may recommend testing for BV in your current pregnancy. Early treatment, ideally before 20 weeks, could reduce the risk of delivering prematurely.
While the exact link between BV and pregnancy complications is not fully understood, there is evidence that BV can increase susceptibility to other sexually transmitted infections (STIs) such as chlamydia and HIV. If you are HIV-positive, BV can increase the likelihood of transmitting HIV to your baby.
Treating BV During Pregnancy
If you are diagnosed with BV, your doctor will likely prescribe antibiotics. These can be taken orally or as a gel inserted into the vagina. If your symptoms are mild or nonexistent, treatment might not be necessary, as BV sometimes resolves on its own. However, if you’ve previously had a premature birth, antibiotics may be recommended even in the absence of symptoms.
The primary antibiotic used for BV, Metronidazole, can cause side effects like nausea and a metallic taste in the mouth. To mitigate these, it’s advisable to take the medication with food. If the tablets cause vomiting, consult your doctor for alternative treatments.
Antibiotics are generally safe during pregnancy and effective in clearing BV infections. However, recurrence is common, with more than half of women experiencing a return of symptoms within three months. This is because antibiotics may disrupt the balance of good bacteria in the vagina. If symptoms persist or return within a month, inform your doctor, who may recommend follow-up testing and treatment.
Another approach to treating BV is using pH-balancing treatments that restore the vagina’s natural acidity, helping good bacteria to thrive. These treatments, typically in gel form, are inserted into the vagina every other evening for at least a month. While not universally effective, they are safe to try and may help prevent recurrent BV.
Preventing BV
Preventing BV is challenging since its exact causes are not well understood. However, certain practices can reduce your risk:
- Use condoms: Particularly with new sexual partners, as sexual activity can alter vaginal bacteria.
- Quit smoking: Smoking increases the risk of BV and is harmful to your baby.
- Practice good hygiene: Wash your genitals with pH-neutral, unscented soap, and avoid douching or using scented products in the genital area.
- Consider vitamin D: While the role of vitamin D in preventing BV is not clear, maintaining adequate levels is essential for overall health during pregnancy. Consult your midwife about taking a 10mcg vitamin D supplement if you’re not already doing so.
By following these guidelines and consulting your healthcare provider, you can manage and reduce the risks associated with bacterial vaginosis during pregnancy, ensuring a healthier outcome for both you and your baby.
Also read: Can You Have a Vaginal Birth with Gestational Diabetes?






