Understanding HIV and AIDS in Pregnancy
Introduction to HIV and AIDS
What is HIV?
HIV, or human immunodeficiency virus, is a virus that attacks the body’s immune system, which is the body’s natural defense against illnesses. Without a strong immune system, the body has trouble fighting off diseases and infections. HIV is most commonly transmitted through the exchange of bodily fluids during sexual contact. It can also be spread through blood, often by sharing needles or drug-injecting equipment, and from mother to child during pregnancy, childbirth, or breastfeeding.
What is AIDS?
AIDS stands for acquired immune deficiency syndrome. It is the most severe stage of HIV infection, where the immune system is badly damaged, and the body becomes vulnerable to opportunistic infections and certain cancers. Thanks to advancements in treatment, reaching this stage is much less common today, especially in places with access to medical care. Many healthcare providers prefer to refer to it as advanced HIV infection or late-stage HIV rather than AIDS.
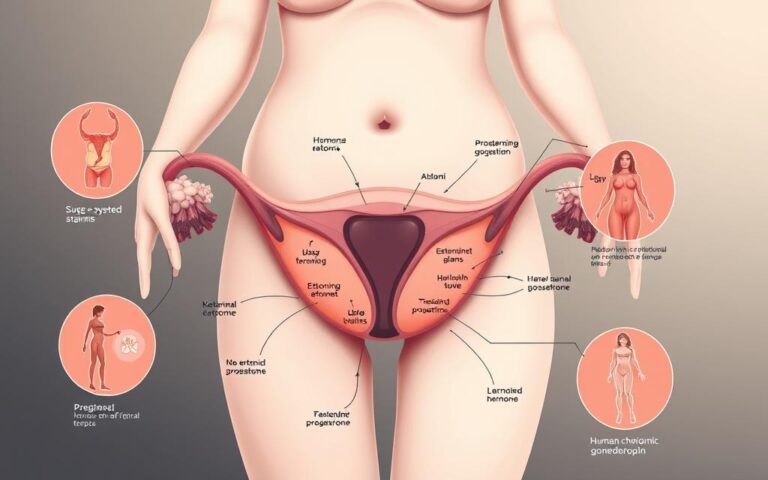
HIV Transmission During Pregnancy
How HIV Affects Pregnancy
HIV can be transmitted from a mother to her baby in three main ways: during pregnancy through the placenta, during childbirth through exposure to maternal blood and fluids, and through breastfeeding. Without treatment, the risk of transmission from mother to child is significant. However, with proper medical care, this risk can be reduced to less than 1%.
Importance of Early Testing
Knowing your HIV status as early as possible in pregnancy is crucial. The only way to confirm if you have HIV is through a blood test. This test is typically offered as part of routine antenatal care. Early detection allows for timely intervention, which can significantly reduce the risk of transmitting the virus to your baby and help maintain your health.
Symptoms and Testing
Recognizing Symptoms of HIV
HIV symptoms can be difficult to recognize, as they often mimic other common illnesses. Many people experience flu-like symptoms two to six weeks after contracting the virus. However, it is also possible to live with HIV for years without exhibiting any symptoms, which is why regular testing is essential, especially if you have risk factors.
The HIV Test Experience
The HIV test is a simple blood test. Your midwife will explain what the test involves and what the possible outcomes are. If you consent, a small blood sample will be taken from your arm and sent to a lab for analysis. While rapid HIV tests are available, the full blood test is considered the most accurate.
Understanding Test Results
Negative Test Result
A negative HIV test result generally means you do not have the virus. However, if you have risk factors or potential recent exposure, a follow-up test might be recommended later in your pregnancy to confirm your status.
Positive Test Result
A positive test result indicates the presence of HIV antibodies in your blood. This can be a challenging diagnosis to process, but early detection allows for effective management. You will be referred to a specialized healthcare team experienced in managing HIV during pregnancy, who will provide both medical care and emotional support.
Managing HIV During Pregnancy
Treatment and Medication
If you are HIV positive, antiretroviral therapy (ART) will be offered. ART can dramatically reduce the viral load in your body, lowering the risk of transmission to your baby. It is essential to adhere to the prescribed treatment plan and attend regular check-ups.
Dealing with Side Effects
ART can cause side effects such as nausea, headaches, and fatigue. While these can be challenging, it’s important to continue taking your medication and discuss any side effects with your healthcare team. They may adjust your treatment to minimize discomfort.
Preparing for Birth
Delivery Options
The method of delivery will be discussed with your healthcare provider, depending on how well your HIV is managed. If your viral load is low, a vaginal birth may be possible. However, if the viral load is high, a cesarean section might be recommended to reduce the risk of transmission.
Post-Birth Care for Your Baby
After birth, your baby will receive antiretroviral medication for a few weeks to further reduce the risk of HIV. They will be tested for HIV several times in the first months of life.
Breastfeeding Considerations
HIV can be transmitted through breast milk, so formula feeding is recommended to prevent transmission. Your healthcare provider will guide you on safe feeding options for your baby.
Getting Support and Information
Support Networks
Organizations like the Terrence Higgins Trust and Positively UK provide invaluable support and resources for individuals living with HIV. They offer counseling, peer support groups, and a wealth of information to help you navigate your journey.
Staying Informed
Reliable information is crucial for managing HIV effectively. Resources such as NAM Aidsmap and NHS Choices offer up-to-date information about HIV and AIDS, treatment options, and living well with the virus.
Conclusion
Managing HIV during pregnancy involves understanding the virus, adhering to treatment, and making informed decisions about your care. With early diagnosis and effective treatment, individuals with HIV can lead healthy lives and have healthy babies.
FAQs
1. Can HIV be completely cured?
No, HIV cannot be cured. However, with proper treatment, it can be managed effectively, allowing individuals to live healthy lives.
2. How often should I get tested for HIV during pregnancy?
You should be tested at your first antenatal visit and may be offered additional tests if you have risk factors or potential exposure.
3. Is it safe to take HIV medication during pregnancy?
Yes, antiretroviral medications prescribed during pregnancy are safe and necessary to reduce the risk of transmission to your baby.
4. What should I do if I test positive for HIV while pregnant?
Seek support from your healthcare provider, who will refer you to a specialist team to manage your care and discuss treatment options.
5. Can I have a vaginal birth if I have HIV?
Yes, if your viral load is low, your healthcare provider may support a vaginal birth. The decision will be based on your individual circumstances.